COMMERCIAL MARKET INTELLIGENCE
PayerPrice Alternatives
PayerPrice offers one approach to solving the price transparency problem, though it's far from the only option. This guide explores the leading alternatives for 2026, what differentiates them, and how to evaluate which platform fits your organization's needs.
The Best Payer Price Alternatives for 2026
Healthcare price transparency data has become a strategic asset, but accessing raw MRF files is only the first step. The real challenge lies in transforming billions of negotiated rates into intelligence you can actually act on.
Why organizations are seeking PayerPrice alternatives
PayerPrice is a price transparency vendor that displays raw negotiated rates directly from insurers' Machine-Readable Files, or MRFs. These MRFs are standardized data files that health plans publish under federal transparency rules, containing the actual rates insurers have negotiated with providers. While PayerPrice gives users access to this pricing data, many organizations find themselves looking for alternatives that go beyond raw data.
The search for alternatives typically comes down to a few key factors:
- Depth of support and knowledge: Price transparency data is complex, with nuances in medical billing codes, rate structures, and payer methodologies that require specialized expertise to interpret accurately
- Limited analytics capabilities: Platforms that simply display raw data without advanced visualizations and AI-powered insights leave users doing extensive manual analysis to extract meaningful intelligence
- Integration gaps: Many organizations struggle to connect price transparency data to their existing enterprise workflows, revenue cycle systems, or contracting processes
The market now offers several robust alternatives, each with distinct strengths depending on whether you're a provider, payer, employer, or MedTech company.
Top PayerPrice alternatives for price transparency data
Gigasheet
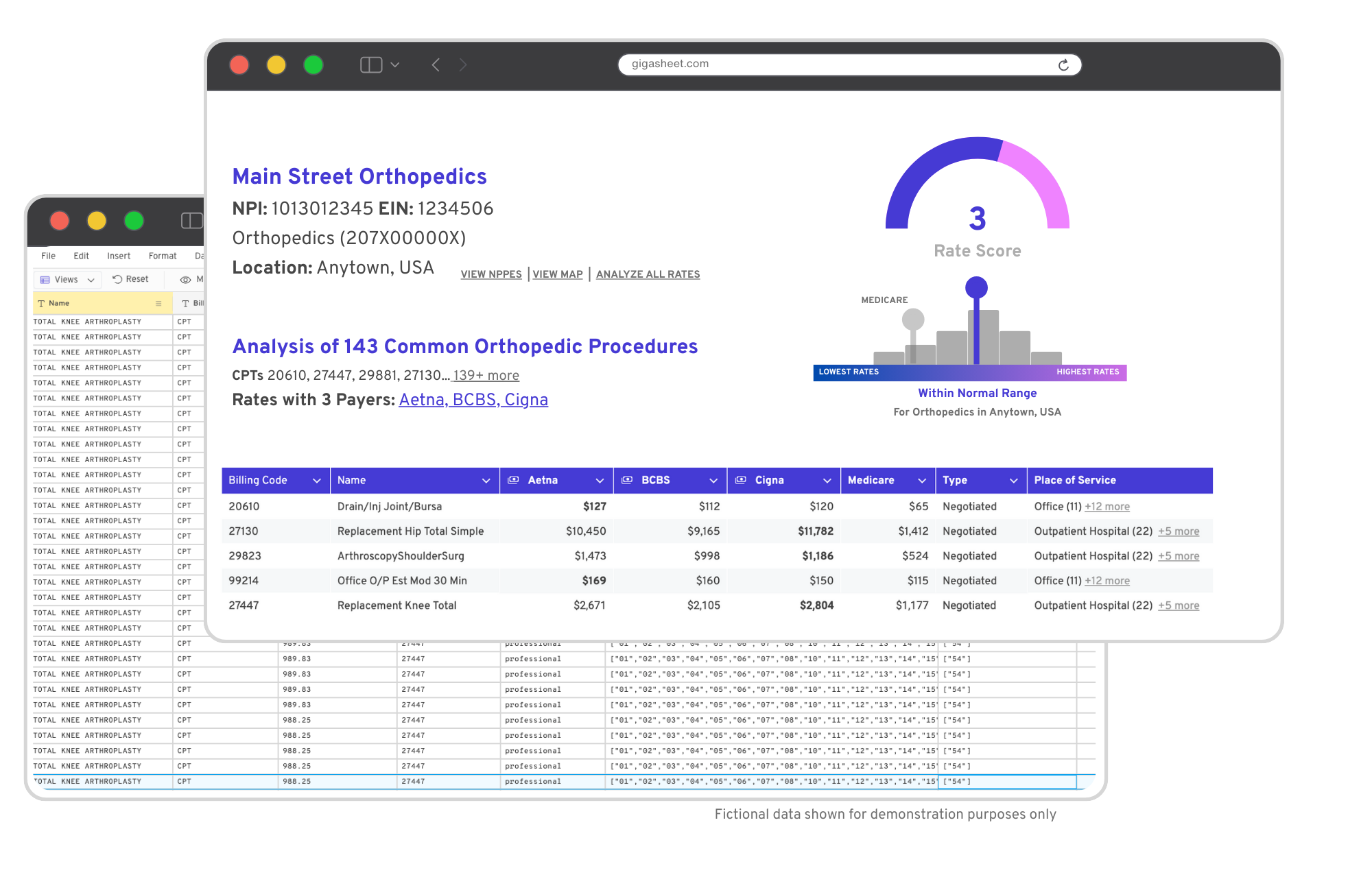
Gigasheet delivers AI-powered healthcare market intelligence that transforms complex price transparency data into actionable insights. Rather than simply displaying raw rates, Gigasheet's proprietary AI models automatically surface outlier rates, contract issues, and market trends. Included Market Intelligence reproting eliminates the manual analysis that would otherwise be required when working with billions of healthcare rates.
What sets Gigasheet apart is its combination of analytical depth and usability. The platform features new advanced visualizations, an intuitive spreadsheet-like interface that lets users drill down from high-level aggregations to row-level details in a single click. Every data point can be traced back to its original MRF source file, which builds confidence in decision-making that raw data displays cannot match.
Gigasheet serves providers, payers, self-insured employers, and MedTech companies. The platform maintains SOC 2 Type II compliance and offers seamless enterprise integration capabilities and a robust API.
Turquoise Health
Turquoise has established itself as a leading platform for tracking negotiated rates across both payer and provider price transparency data. Their Price Relativity Index offers an alternative benchmarking methodology to traditional percent-of-Medicare comparisons, which has been the industry standard for years. However, most tools now integrate Medicare benchmarks and it's become industry standard.
The platform also supports percent of cohort analysis, allowing users to compare rates against market peers rather than just Medicare baselines. Turquoise serves a broad range of healthcare stakeholders and has built significant market presence since transparency regulations took effect. Cost should certainly be a consideration when assessing Turquise as many solutions include a hefty consulting services component.
Serif Health
Serif Health focuses on aggregating and normalizing price transparency data to make it more accessible for healthcare organizations. Their approach emphasizes data quality and standardization across the fragmented landscape of payer-published files.
The platform helps users navigate the inconsistencies that often plague raw MRF data. However, organizations seeking automated insight generation may find they still require additional analytical tools to complement Serif's offerings.
Clarify Health
Clarify Health combines claims data with price transparency information to provide a more comprehensive view of healthcare economics. This multi-source approach can reveal patterns that pricing data alone might miss, such as how negotiated rates translate into actual utilization and spending.
Their analytics platform serves health systems and payers looking to understand both what rates are negotiated and how those rates play out in practice.
H1 (fka Ribbon Health)
H1 approaches price transparency through the lens of provider data and healthcare navigation. Their cost transparency tools help organizations understand pricing in the context of provider networks and care pathways.
The platform is particularly relevant for organizations focused on steering patients toward high-value care options based on both quality and cost considerations.
Trilliant Health
Trilliant Health offers market analytics and healthcare intelligence that extends beyond price transparency into broader strategic planning. Their platform helps organizations understand competitive dynamics and market positioning.
For users whose primary focus is rate benchmarking and contract negotiation, Trilliant's broader market scope may be more than necessary. That said, it provides valuable context for strategic decisions.

How to compare healthcare price transparency vendors
Choosing the right platform requires evaluating several dimensions beyond data access alone. Here's what matters most when comparing your options.
Data coverage and rate granularity
The value of any price transparency platform depends on how comprehensively it captures the market you care about. NPI-level rate access, meaning rates tied to specific provider identifiers, allows for precise benchmarking. The ability to compare across multiple payers and geographic regions adds another layer of analytical power.
Some platforms excel in certain markets or payer types while having gaps in others. It's worth asking vendors specifically about coverage for your priority payers and service areas before committing.
AI-powered analytics and automated insights
There's a meaningful difference between platforms that display raw data and platforms that automatically surface what matters. AI-powered analytics can identify outlier rates, flag potential contract issues, and reveal market trends without requiring manual queries across massive datasets.
When you're processing billions of rates across thousands of contracts, manual analysis at that scale simply isn't practical. The distinction between "here's all the data" and "here's what you should look at" often determines whether insights actually reach decision-makers in time to act on them.
Vendor alignment and market neutrality
Some vendors serve only providers, while others work with both providers and payers. This distinction matters because it affects data exclusivity and potential conflicts of interest.
Consider whether your vendor's customer base creates any competitive concerns for your organization. A platform that serves both sides may offer broader market intelligence, though it could raise questions about how data is shared or used.
Enterprise integration and workflow support
Price transparency insights are most valuable when they flow into your existing decision-making processes. API access, system compatibility, and the ability to embed real-time payer data into revenue cycle or contracting workflows all reduce the friction between insight and action.
Platforms with strong integration capabilities make it easier to operationalize what you learn from the data.
Security compliance and data protection
Enterprise healthcare organizations require robust security standards. SOC 2 Type II compliance has become a baseline expectation, though it's worth verifying each vendor's specific certifications and data handling practices.
Traceability to original MRF source files
When you're making contract decisions based on market data, you want confidence that the underlying information is accurate. The ability to trace any rate back to its original insurer-published file provides an audit trail that supports defensible decision-making.
Traceability also helps when rates seem anomalous. You can verify whether the issue lies in the source data or in the platform's interpretation of that data.
Key use cases for price transparency solutions
Contract negotiation and rate benchmarking
The most common application is using transparency data to inform managed care contract negotiations. With market-backed rate intelligence, providers can demonstrate where their rates fall relative to competitors and make evidence-based cases for adjustments.
Payers similarly use this data to understand their competitive position and identify opportunities for network optimization.
Network optimization and provider prospecting
Fee schedule analysis reveals opportunities beyond existing contracts. Organizations can identify providers with favorable rate structures for network expansion, or spot markets where their rates create competitive advantages.
Competitive market intelligence for MedTech
Medical device and healthcare technology companies increasingly use pricing data to understand how their products are reimbursed across different payers and markets. This intelligence informs pricing strategy, market positioning, and sales targeting.
What AI-powered analytics means for price transparency tools
AI-powered analytics in this context refers to automated systems that process massive datasets to surface meaningful patterns without manual intervention. Rather than requiring users to formulate queries and interpret results, platforms with AI capabilities proactively highlight what deserves attention.
Key capabilities include:
- Outlier detection: Automatically flags rates that deviate significantly from market norms, helping identify both opportunities and potential data quality issues
- Contract issue identification: Surfaces potential problems in payer agreements, such as rates that don't match expected fee schedules or unusual payment terms
- Trend analysis: Reveals market pricing patterns over time without requiring manual querying across historical data
The practical impact is substantial. When working with billions of rates, the difference between passive data access and active insight delivery determines whether organizations can actually use what they're paying for.
Price Transparency Market Intelligence

Hands-on Support Included
Gigasheet includes analytic and technical support with every package. Executive Market Intelligence reports are tailored to clients requirements.

Analytics & Data In One
Gigasheet includes analytic and technical support with every package. Executive Market Intelligence reports are tailored to clients requirements.

AI & API
Gigasheet's AI powered analytics save time and manual sifting. Best of all data and analytic insights are available via an API for direct integration.











