Healthcare
Price Transparency Data Reveals the Real Story Behind Capital Women's Care vs UnitedHealthcare Contract Battle

On August 1, 2025, Capital Women's Care (CWC), one of the largest OB/GYN practices in the Mid-Atlantic region went out-of-network with UnitedHealthcare, affecting tens of thousands of women across Maryland, Virginia, Pennsylvania, and Washington D.C. The contract dispute between Capital Women's Care (CWC) and UnitedHealthcare offers a fascinating case study in how price transparency data can illuminate the real dynamics behind these high-stakes negotiations.
The Public Battle
Capital Women's Care, with more than 250 physicians and healthcare professionals, confirmed that its agreement with UnitedHealthcare would lapse despite ongoing negotiations. The practice urged patients to contact UHC to voice their concerns about losing access to their providers.
UnitedHealthcare fired back with detailed public claims on their website, alleging that CWC "refused to move off its demands for double-digit price hikes" and is "significantly higher cost today compared to peer providers throughout Maryland and Virginia". UHC provided specific examples, claiming that a vaginal delivery from CWC would cost "more than 120% higher – or over $2,600 more – than the average cost of other OB/GYN providers".
But what does the actual price transparency data reveal about these competing claims?
What the Transparency Data Shows
Using Capital Women's Care's negotiated rates from UnitedHealthcare's own machine-readable files, we analyzed a sample of common OB/GYN procedures from Maryland rate data. While this represents only a subset of all procedures and focuses specifically on Maryland rates, it provides valuable insights into the real payment dynamics between these organizations. The data paints a more nuanced picture than either party's public statements suggest.
Data Methodology Note: Our analysis examined negotiated rates for Capital Women's Care from publicly available machine-readable files, focusing on Maryland providers and filtering out statistical outliers (rates below 50% or above 500% of Medicare). We analyzed rates for both UnitedHealthcare and CareFirst across three common OB/GYN procedures where both payers had sufficient data.
CWC's Rate Position vs Other Payers
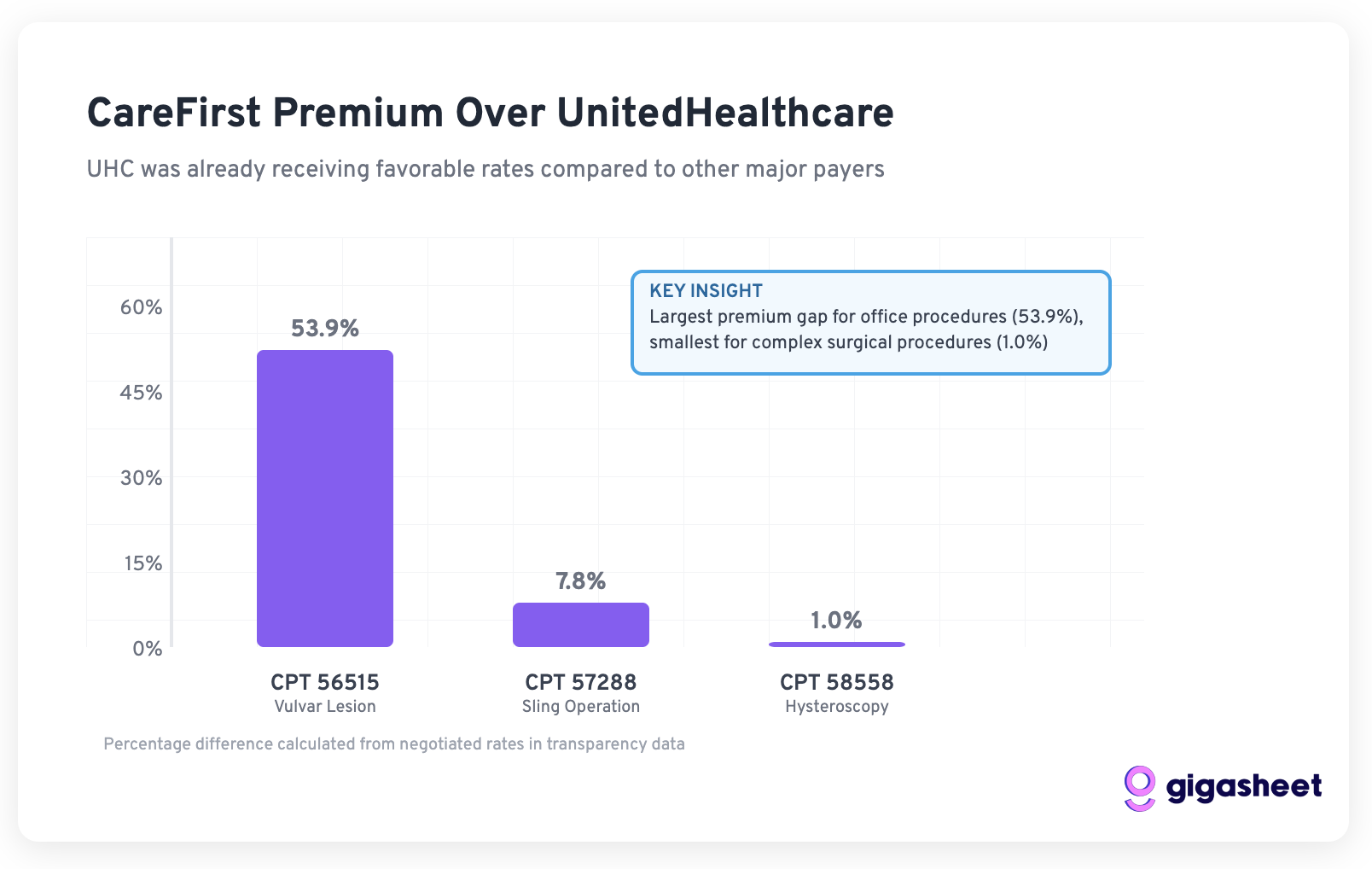
Our analysis of three common OB/GYN procedures in Maryland reveals that CWC's rates with UnitedHealthcare were actually quite competitive compared to other major payers:
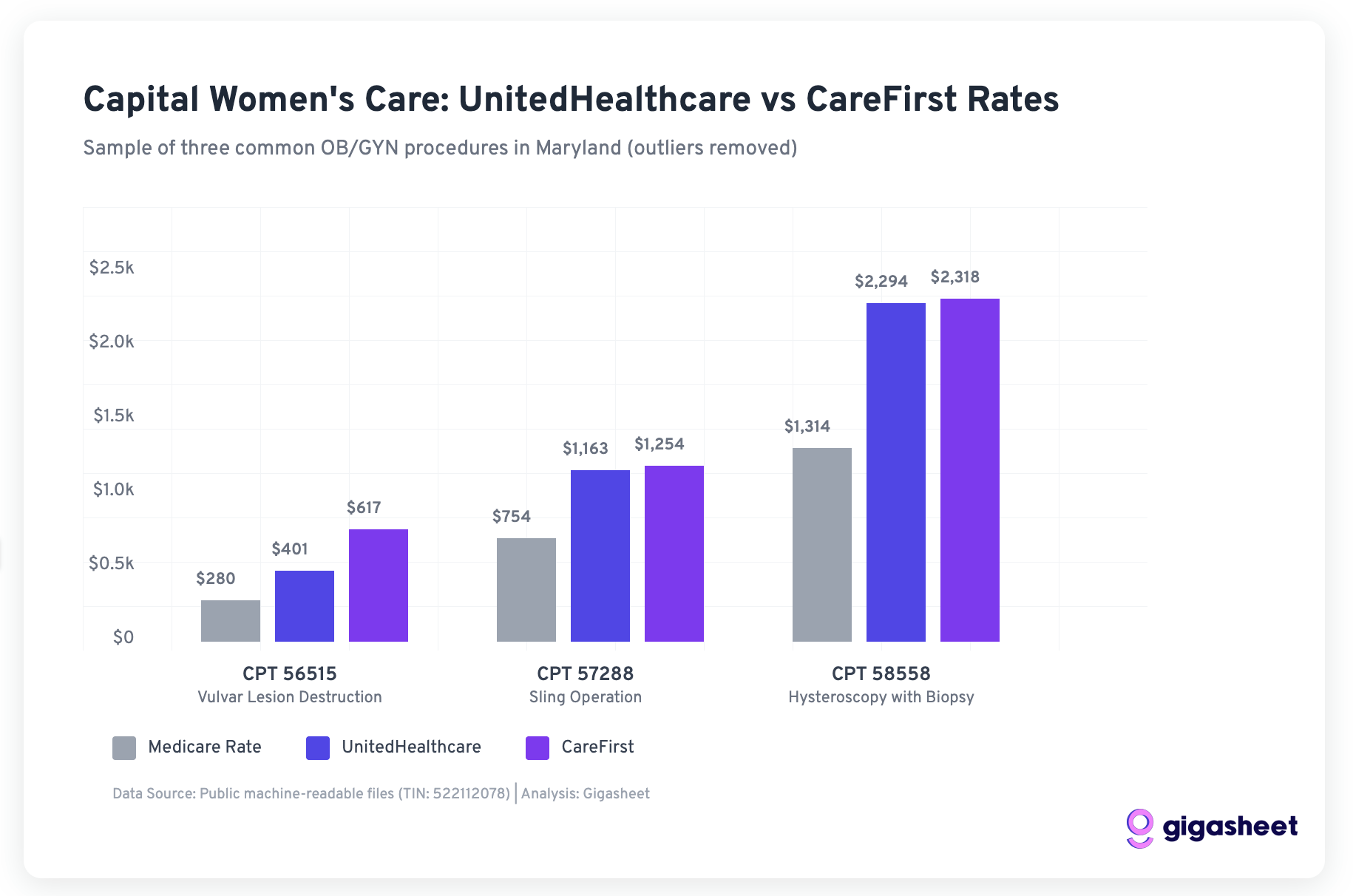
For the three procedures where both UHC and CareFirst have negotiated rates with CWC:
- CPT 56515 (Vulvar Lesion Destruction): UHC paid $401 vs CareFirst's $617 (53.9% difference)
- CPT 57288 (Sling Operation): UHC paid $1,163 vs CareFirst's $1,254 (7.8% difference)
- CPT 58558 (Hysteroscopy): UHC paid $2,294 vs CareFirst's $2,318 (1.0% difference)
This sample data suggests UnitedHealthcare was already getting favorable rates from CWC compared to other major payers, calling into question UHC's claims about CWC being "significantly higher cost."
The Medicare Benchmark Reality
Both UHC and CareFirst were paying CWC rates well above Medicare in our sample:
- UnitedHealthcare: 143-175% of Medicare rates
- CareFirst: 166-220% of Medicare rates
While CareFirst paid higher rates, UnitedHealthcare's rates were still substantial premiums over government reimbursement, suggesting the "double-digit increases" CWC requested may have been attempts to align with market rates other payers were willing to pay.
Important Limitation: This analysis is based on a sample of three procedures in Maryland only. A comprehensive analysis would require examining all procedure codes across all markets where CWC operates to fully validate these patterns.
The Strategic Context: Market Share Matters
Understanding why CWC might have walked away requires examining UnitedHealthcare's position in the Maryland market. According to KFF data, UnitedHealthcare holds only 9% of Maryland's large group market share as of 2023. This relatively small market position gave CWC significant leverage.
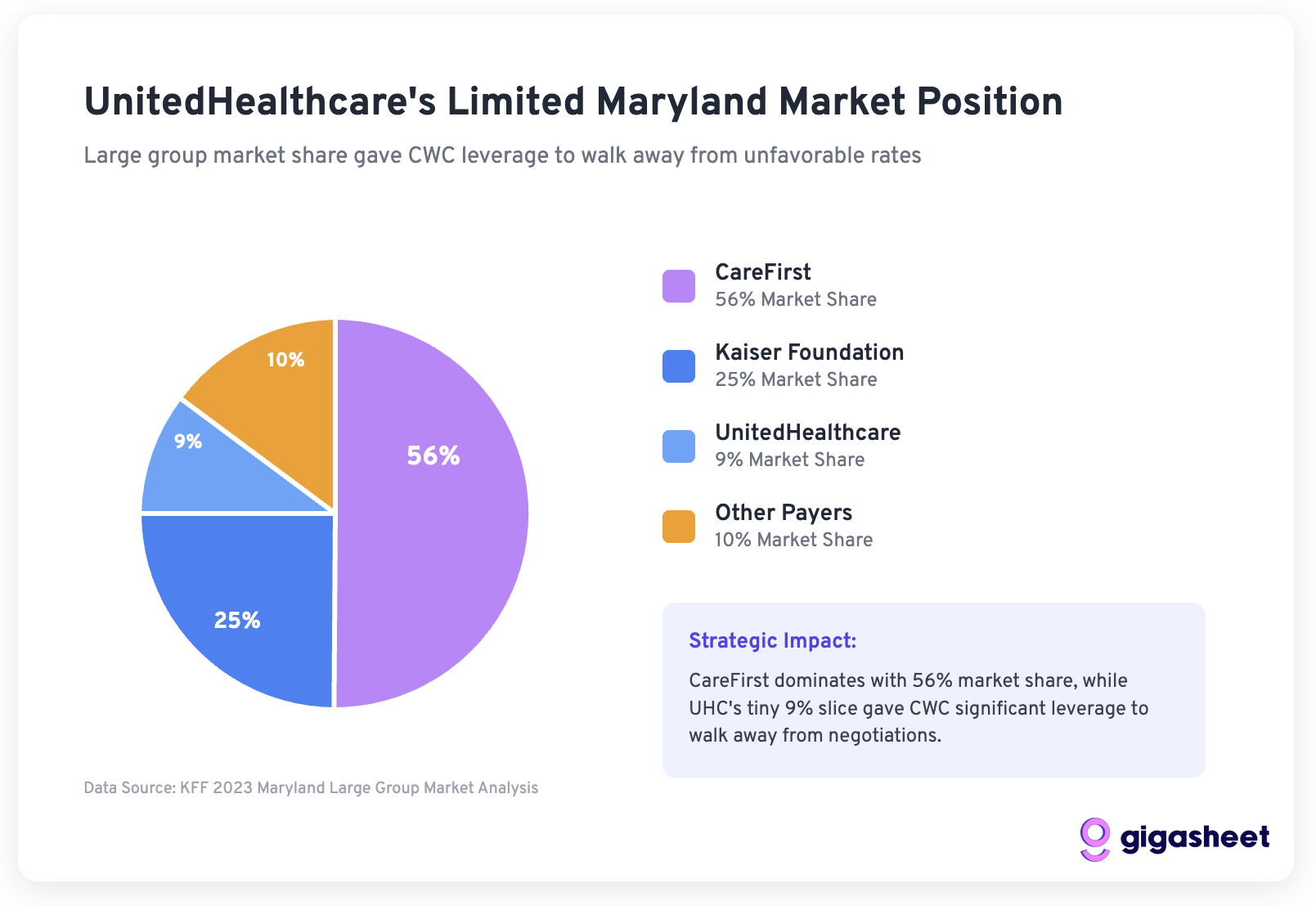
The Math of Walking Away:
- UHC represents a small portion of CWC's patient base
- CWC has contracts with larger payers (Aetna, CareFirst, Cigna) paying higher rates
- The practice serves over 250 providers across multiple states
- Walking away from 9% of the market to establish rate precedent makes strategic sense
Evaluating UnitedHealthcare's Public Claims
UHC's website makes several specific claims that we can evaluate against transparency data:
Claim 1: "CWC is significantly higher cost compared to peer providers"
Assessment: Partially Misleading
While CWC may charge more than some providers, our analysis shows UHC was paying competitive rates compared to other major payers for the same services. The "peer provider" comparison lacks context about geographic market rates and provider quality differences.
Claim 2: "Double-digit price hikes that would make them 30% higher than average"
Assessment: Missing Context
This claim doesn't account for:
- How UHC's current rates compared to other payers
- Whether the "average" includes lower-quality or differently positioned providers
- Regional cost variations in the expensive Mid-Atlantic market
Claim 3: Specific procedure cost comparisons
Assessment: Potentially Accurate but Incomplete
UHC's claims about delivery costs may be accurate, but they don't provide the full market context. The transparency data shows significant rate variation across payers and procedures, suggesting that "expensive" is relative to the comparison set chosen.
How Price Transparency Changes the Game
This dispute illustrates how price transparency data is reshaping healthcare negotiations in several ways:
Informed Leverage
Providers like CWC can now see exactly how their rates compare across payers, enabling more strategic negotiations. CWC knew they were giving UHC favorable rates compared to CareFirst.
Public Accountability
Both parties made public claims that can now be fact-checked against actual negotiated rates. UHC's claims about CWC being "significantly higher cost" are more nuanced when viewed against the full payer landscape.
Market Benchmarking
The transparency data reveals that:
- Regional markets have substantial rate variations
- Provider quality and market position justify rate premiums
- "Expensive" is relative to the comparison being made
Strategic Positioning
For a practice with CWC's market position, maintaining rate discipline across payers becomes crucial. Accepting below-market rates from one payer can undermine negotiations with others.
The Real Winner: Market Transparency
While patients are caught in the middle of this dispute, the broader healthcare market benefits from the transparency this conflict provides. The public availability of actual negotiated rates means:
- Patients can make more informed choices about providers and plans
- Employers can better evaluate insurance plan value propositions
- Providers can benchmark their rates against actual market data
- Payers must justify rate decisions with real data rather than selective comparisons
Looking Forward: Lessons for Healthcare Negotiations
The CWC-UHC dispute offers several lessons for future healthcare contract negotiations:
- Price transparency data is now a negotiating tool - Both sides can and will use actual rate comparisons to support their positions
- Market share matters in rate negotiations - UHC's 9% Maryland market share limited their leverage against a large, established provider
- Public relations battles require data backing - Claims about "expensive" providers can now be fact-checked against actual negotiated rates
- Provider consolidation creates negotiating power - Large practices like CWC can afford to walk away from unfavorable contracts
The Path to Resolution
For this specific dispute, the transparency data suggests both parties have reasonable positions:
- CWC was indeed giving UHC favorable rates compared to other payers, justifying their request for increases
- UHC faces pressure to control costs for members while maintaining an adequate provider network
A resolution likely requires:
- UHC acknowledging that their current rates were below market
- CWC accepting that dramatic rate increases affect patient costs
- Both parties finding middle ground that reflects true market positioning
The availability of actual negotiated rate data should, in theory, make these conversations more productive by establishing shared facts about market rates and provider positioning.
Conclusion
The Capital Women's Care vs UnitedHealthcare contract dispute demonstrates how price transparency is fundamentally changing healthcare negotiations. While both parties made public claims supporting their positions, our analysis of actual negotiated rate data from Maryland reveals a more complex story where market dynamics, strategic positioning, and regional factors all play crucial roles.
Key takeaways from our data analysis:
- UHC was paying competitive rates compared to other major payers for the procedures we examined
- CWC's decision to walk away makes strategic sense given UHC's limited 9% Maryland market share
- Both payers were paying well above Medicare rates, suggesting room for negotiation
Important caveats: Our analysis examined only three common procedures from Maryland data. A comprehensive evaluation would require analyzing all procedure codes across all markets where CWC operates to fully validate these patterns.
As more stakeholders gain access to this previously hidden pricing information, we can expect healthcare contract negotiations to become more data-driven, transparent, and ultimately more rational. The real winners will be those who can effectively analyze and act on this new transparency to make better decisions about healthcare coverage, provider selection, and contract terms.
For healthcare organizations navigating similar negotiations, tools like Gigasheet make it possible to analyze massive price transparency datasets and understand true market positioning - turning transparency requirements from compliance burden into competitive advantage.
The ease of a spreadsheet. The power of price transparency.






.png)









