Healthcare
Price Transparency Applications for Managed Care: Turning Data Into Strategic Advantage
.png)
Price transparency rules from CMS have permanently changed how managed care organizations (MCOs), hospital managed care teams, and provider networks approach contracting. Negotiated rate data that was once locked away is now published in massive machine-readable files (MRFs) that cover nearly every payer and provider nationwide. While the data is far from perfect, it's proven to be a valuable tool in understanding healthcare markets.
For those of us who work in managed care, this represents both an opportunity and a challenge. On one hand, we finally have visibility into competitive reimbursement rates. On the other, these files are massive, messy, and difficult to analyze with traditional tools.
In this post, we’ll explore how managed care leaders are applying price transparency data and how Gigasheet’s intuitive interface enables quick, flexible analysis of MRFs. This helps teams move faster at the negotiating table, support smarter network design, and strengthen payer-provider relationships.
How Managed Care Teams Leverage Price Transparency Data
Price transparency is not just about compliance. For managed care teams, it is a way to balance cost, quality, and access with evidence. With payer and hospital transparency data, teams can:
- Benchmark reimbursement rates for key CPT, HCPCS, and DRG codes across payers and providers in a given market
- Support rate negotiations with market evidence when payer or hospital proposals deviate from local norms
- Identify outlier rates that could be renegotiation targets
- Assess reimbursement trends across geographies, plan types, or service settings
- Guide network strategy by evaluating which payers, providers, or service lines represent the best value for high-volume procedures
For hospital managed care teams, this data helps leadership align around a fact-based view of competitiveness. For MCOs, it provides insight into which providers to include in networks and how to structure sustainable contracts.
The Scale Problem: Billions of Rows, Limited Time
If you have ever opened an MRF (the giant JSON files payers are required to publish), you know the reality. They often contain billions of rows, multiple plan variations, nested structures, and inconsistent naming conventions. Many vendors respond by selling a static database of extracted rates. While that can give you access to the numbers, it locks you into predefined queries and limited ways of looking at the data.
Managed care teams need more than a simple database lookup. When preparing for contract negotiations or assessing payer proposals, speed and flexibility matter. You should be able to pivot perspectives, test hypotheses, and follow threads in the data in real time. Gigasheet makes that possible with a spreadsheet-style interface that allows direct exploration of the transparency data, not just someone else’s curated slice.
Gigasheet: A Big Data Spreadsheet for Managed Care
Gigasheet removes the barriers by providing a spreadsheet interface designed for massive datasets. Managed care teams can work with transparency in coverage data directly instead of relying on static reports or clunky interaces.
With Gigasheet, teams can:
- Filter by CPT, DRG, HCPCS, NPI, payer, or provider in seconds
- Switch perspectives between payer and hospital views, commercial and ASO plans, or in-network and out-of-network contracts within the same dataset
- Group and pivot instantly to benchmark by payer, facility, or specialty
- Combine payer and hospital files with claims, utilization, or census data to see your exposure in context
- Ask plain-language questions with AI, such as “What is the average rate for colonoscopies in Virginia across United, Aetna, and Anthem?”
This flexibility means managed care leaders can explore transparency data directly instead of waiting for analysts.
Real Applications for Managed Care Teams
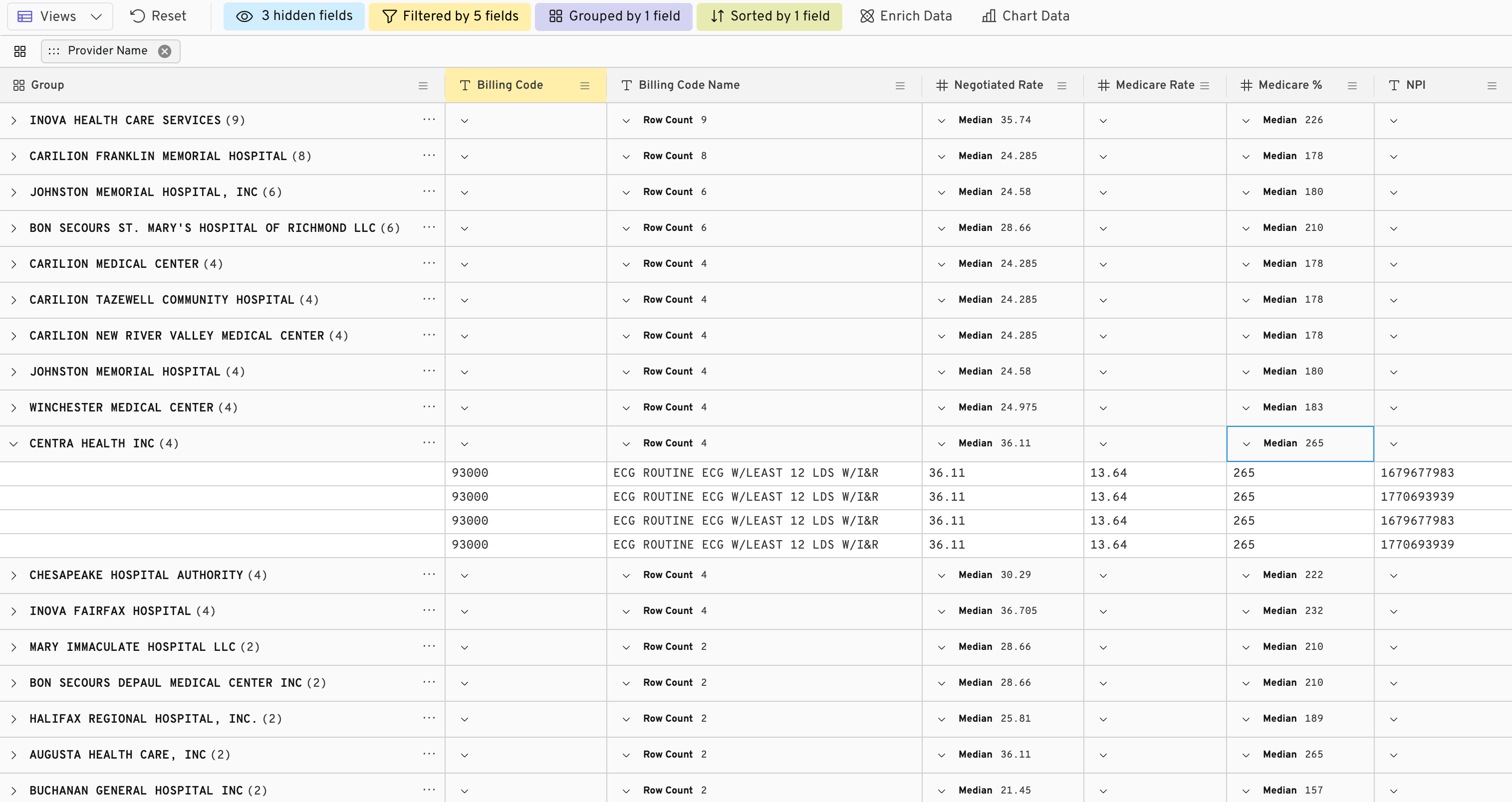
1. Rate Benchmarks for Negotiations
A hospital system preparing to renegotiate cardiology contracts analysis Gigasheet. By grouping negotiated rates by payer and CPT code, they identify which rates are above local averages and bring evidence-based counter-proposals to the table.
2. Market Entry Analysis
An MCO entering Virginia can scan transparency files across all major payers. They focus on high-volume procedures such as childbirth and orthopedics to quickly understand reimbursement dynamics before starting provider outreach.

3. Provider Recruitment and Network Expansion
A health system planning to expand its specialty network can analyze how payers reimburse targeted providers. Side-by-side comparisons in Gigasheet highlight which partnerships are most competitive and sustainable.
4. Cross-Payer Comparisons
Managed care teams often need to compare reimbursement across multiple payers for the same service. In Gigasheet, you can pull hip replacement rates from UnitedHealthcare, Aetna, and Anthem in Virginia and see not only averages but also the range of negotiated variance.
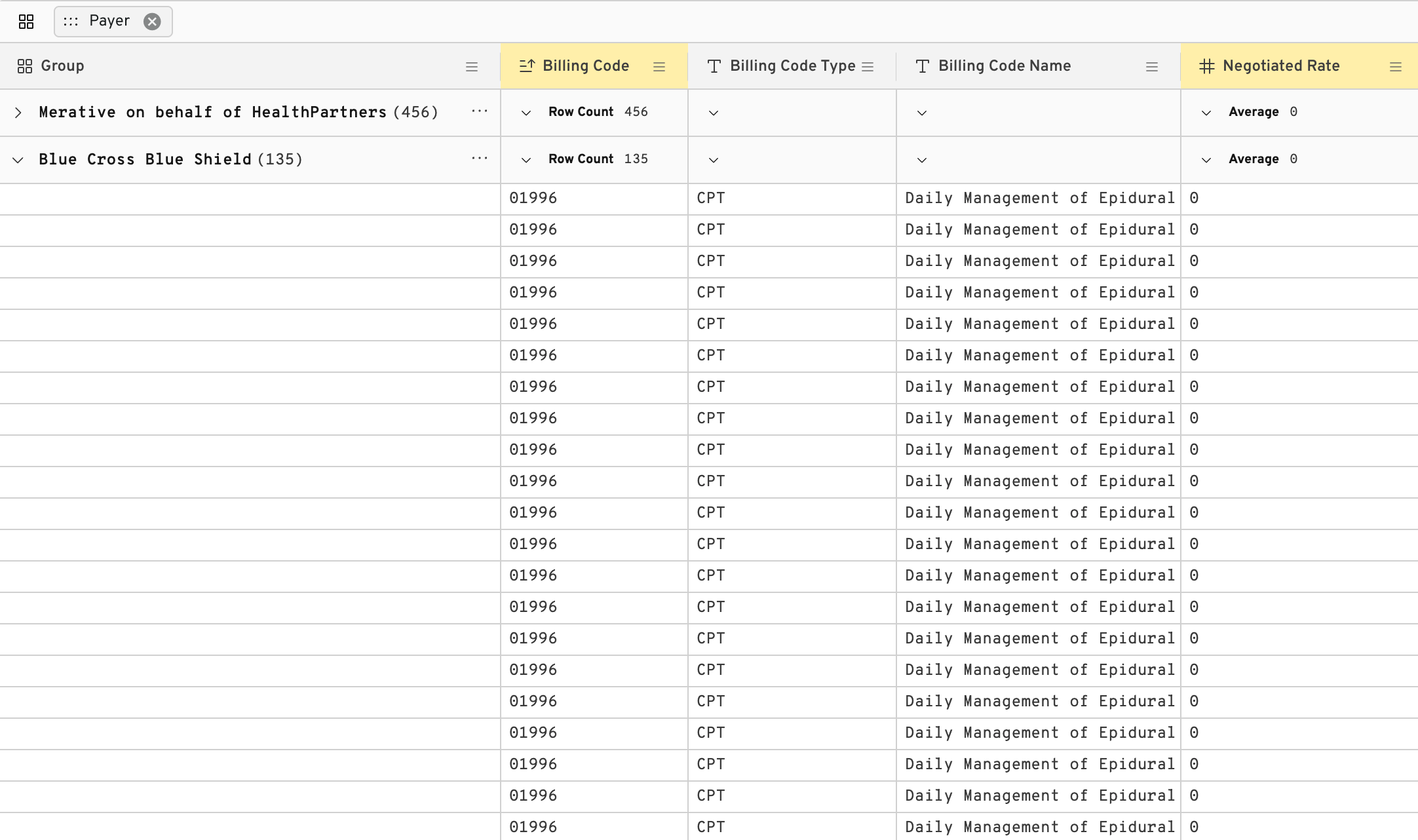
5. Outlier Detection and Compliance
Transparency data frequently contains “zombie” rates that are no longer active or are irrelevant. Gigasheet’s filtering and AI-assisted analysis make it easy to flag these values so teams focus on the data that truly matters.
Overcoming Common Barriers
Some managed care leaders hesitate to use transparency data because they assume the only option is to buy a pre-extracted database of rates. While those products can give access to the numbers, they often come with real limitations. Gigasheet takes a different approach:
- File size: Instead of selling a static extract, Gigasheet ingests the full MRF and handles billion-row datasets directly.
- Data cleanup: Our algorithms flag zombie rates but always preserve raw row-level details, so you know exactly what came from the original file.
- Ease of use: You are not locked into canned queries or predefined dashboards. The spreadsheet-style interface is familiar to any Excel user and supports true exploration.
- Integration: Rather than a siloed rate database, Gigasheet lets you combine payer and hospital transparency data with your own claims and utilization data for context.
The result is more than just access to data. Managed care teams gain the speed and flexibility to explore, benchmark, and negotiate with confidence.
From Data to Decisions
Price transparency has shifted managed care into a new era. Instead of operating in the dark, teams can quantify how contracts compare to the market. The real advantage comes from being able to apply that insight in real time.
With Gigasheet, managed care leaders can:
- Enter payer negotiations with market-wide benchmarks
- Justify network strategies with hard evidence
- Empower leadership with fact-based intelligence instead of anecdote
- Explore multiple perspectives on the same dataset without delays
Transparency data is no longer just a compliance exercise. It is a competitive advantage.
Final Thought
Managed care will always focus on balancing cost, quality, and access. Price transparency data strengthens that mission by giving teams sharper tools.
By pairing these datasets with an intuitive interface like Gigasheet, managed care teams can move at the speed of business: exploring, benchmarking, and negotiating with facts in hand.
The future of managed care is not about waiting for reports. It is about turning transparency into strategy.
The ease of a spreadsheet. The power of price transparency.






.png)









